In June 2022, three HQC staff and board members travelled to Gothenburg, Sweden to attend the International Forum on Quality and Safety in Healthcare. The conference is an international knowledge hub for excellence in patient safety and health care improvement, and has been held for over two decades.
After the conference, the HQC team travelled to Copenhagen, Denmark to meet with stakeholders from local health organizations (including Healthcare Denmark, the Danish Health Authority, the Danish Society for Patient Safety and KOMBIT (a non-profit technology organization and health-care partner). The team gained valuable insight into both the Danish model of care for older adults, as well as innovations used within the health sector to support aging adults.
As quality improvement leaders (QI) in Saskatchewan, our work often involves shining a light on best practice, learning from other high-performing systems and trying it in our own backyard. Here, CEO Tracey Sherin and researcher Suelen Meira Goes reflect on their learnings and experiences on the other side of the globe.
Table of contents
- We are all Esther (Suelen)
- Established QI during the UK COVID-19 response (Tracey)
- PDSA cycles in problem-solving (Tracey)
- The triangle of trust (Suelen)
- Change concepts and mental health (Tracey)
- Health supports for an aging population (Suelen)
- As long as possible in your own home (Tracey)
- A Danish approach to workforce shortages (Suelen)
- Conclusion (Tracey and Suelen)
1. We are all Esther (Suelen)
On my first day at the conference, I had the opportunity to visit the Qulturum Center for Learning and Innovation in Healthcare in the Region Jönköping County, about two hours southeast of Gothenburg. Qulturum is engaged in several improvement activities—locally, regionally, nationally and internationally.

They focus on developing improvement knowledge and innovation in health care concerning co-production, patient involvement, cooperation, flow, inter-professional teams, leadership, management and the design of health care. I would say Qulturum is the Swedish version of our Saskatchewan Health Quality Council!
During this visit, I learned how the county combines person-centred and integrated care to put the patient and community at the heart of everything they do. They focus on improving care coordination and the experiences of patients through the Esther model, created in the county and composed of patients, caregivers, providers, and families who work to promote and improve complex care. Esther is a symbolic person, with complex care needs who requires the coordination and integration between the hospital, primary care, home care and community care.
What I could see is that Esther is at the centre of all their daily work—the phrase “What is best for Esther?” serves as a guidepost for QI. This is a good example of both individualized (shared decision-making, case management, personalized medicine) and standardized (guidelines, disease management programs) care.
2. Established QI during the UK COVID-19 response (Tracey)
In the paper “Quality improvement at times of crisis,” Dr. Amar Shah and his colleagues reported on the experience of health system staff in the United Kingdom in using QI tools and processes to respond to the COVID-19 pandemic. The team reported on their findings at the conference in Gothenburg. They found that organizations that had previously established QI “muscle” were more easily able to take advantage of the tools to respond to the challenges they faced.

We saw this in Saskatchewan as well – QI tools like the plan, do, study, act (PDSA) cycle, process mapping, measurement, and driver diagrams were used extensively to design and adapt processes in response to COVID-19.
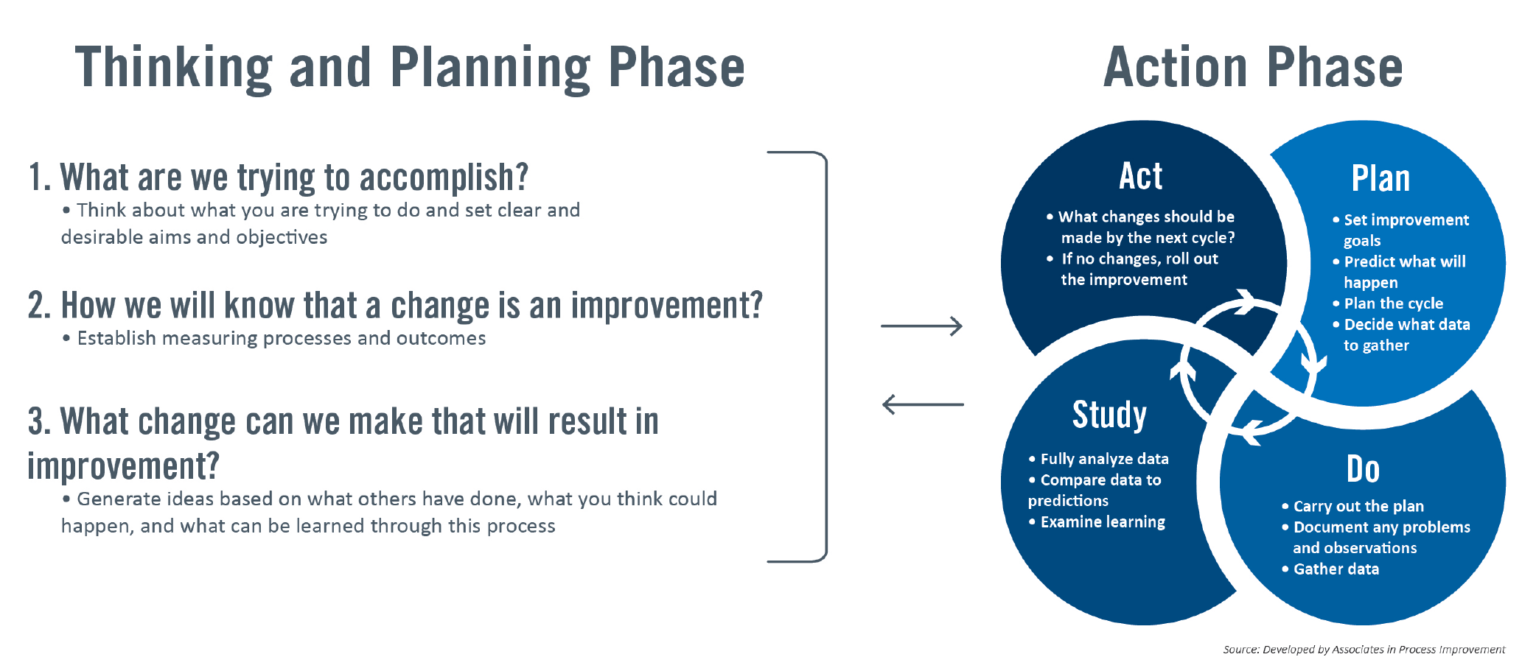
3. PDSA cycles in problem-solving (Tracey)
The PDSA cycle – a four-step method for testing a change by planning it, trying it, observing the results, and acting on what is learned – has proven to be a useful tool to solve complex problems. The COVID-19 pandemic presented a series of new challenges and problems to solve, and the PDSA cycle proved adept at helping teams address those challenges.
One interesting example that the researchers shared: a team was trying to figure out how to safely, effectively, and efficiently use ultraviolet light to disinfect protective hoods worn by staff (which consist of a helmet, face shield, and neck cape). The challenge? To enable proper disinfection, the hoods needed to be rotated constantly. But how do you do that with multiple hoods simultaneously? Through trial and learning, the team discovered that if they hung the hoods from disco ball motors, they would rotate at the right speed!
The next hurdle? Even with proper rotation, the hoods were still not getting clean. They needed to be tipped at an angle to get the ultraviolet light into all the nooks and crannies that needed cleaning. Tipping the hoods at a 45-degree angle seemed to solve the problem, but the challenge again was how could this be done with multiple hoods simultaneously? Through more trial and learning, they found a solution: hanging bags of dry basmati rice to the bottom of the hood would tip it and hold it at the appropriate angle for the disinfection process.

The use of a structured approach to experimentation – the PDSA cycle – allowed the team to quickly test and learn to solve problems.
4. The triangle of trust (Suelen)
One of my favorite keynotes at the conference was delivered by Dr. Kedar Mate, president and CEO at the Institute for Healthcare Improvement (IHI). His speech was a very powerful way to kick off the next two days of learning. Dr. Mate highlighted some important reflections for our health system recovery action plans: Listen to the ones receiving the care and to the ones providing the care.
In addition to sharing stories of burnt-out health providers thinking of leaving their profession, he also showed examples of health-care inequities and disparities that make it difficult for marginalized groups to access medical treatment. These stories show the lack of trust in the system for providers and patients alike. For any system recovery to happen we need to rebuild this trust. The trust triangle was presented as an approach that could be used.
According to this approach, trust has three drivers: authenticity, logic and empathy. When trust is lost, it can almost always be traced back to a breakdown in at least one of them. To build trust, we first need to figure out which driver we “wobble” on.
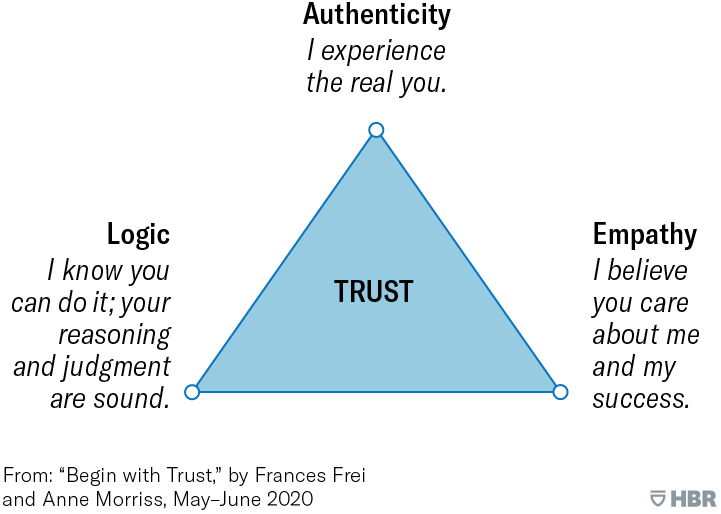
I would say that across the world, we are seeking a radically different health and care system for the future: one that promotes health, addresses health inequity, and regards patients and families as equal members of the care team. This means confronting some big dilemmas at the heart of change; building new structures yet giving people power and autonomy; standardizing care, yet personalizing care; creating small changes that add up to big changes. Thus, it is vital to include the community and health providers in the planning and implementation of actions as well as to document/collect data throughout this process.
5. Change concepts and mental health (Tracey)
To improve mental health at a population level, consider the following change concepts shared by Dr. Amar Shah, from the East London National Health Service (NHS) Foundation Trust: design at scale, test and involve people locally; start by understanding what matters, and what contributes to good mental health and quality of life; understand local assets; partner; test ideas and iterate; move the money (microgrants and funding for local projects); prioritize children; redesign through coproduction.

Learn more about the improvement work that the East London NHS Foundation Trust is doing.
6. Health supports for an aging population (Suelen)
Like many other countries, the Danish care sector is also feeling the pressure of demographic change. Over the past 25 years, Denmark has transformed its health-care structure to implement initiatives specifically for older adults.
Denmark has continuously sought innovative solutions to meet this challenge in collaboration with the community, enabling initiatives that are sustainable, viable and do not compromise the quality of care. I would describe the Danish older adult care model as having three core elements:
People-centred
The Danish health system works with targeted efforts for older adults to be able to maintain their independence and stay in their own homes for as long as possible. Denmark focuses on older adults’ dignity, involvement and empowerment.

Innovations are led by the community, interdisciplinary care providers, and policy-makers, and have a proactive and preventative framework focused on people-centred care, prevention and rehabilitation.
Engaged in multi-sectoral collaboration
There is inter-sectoral collaboration in health and social service delivery. The sectors remain formally autonomous but form a relationship for a common goal or purpose: to improve functional outcomes, quality of life and quality of care for older adults.

For example, health and support services work together while developing innovative reablement services and programs, such as preventative home visits (see point #7). These facilitate older adults living with, or at risk of frailty to restore, improve, and maintain physical and mental function to perform their daily activities. Health and support services focus on doing things in cooperation with individuals rather than doing things for individuals. The reablement can range from physical rehabilitation after spinal surgery to coaching someone on how to cook more nutritious food at home or vacuum their home.
Involving three levels of government
Denmark’s public health care operates within three levels: national, regional, and municipal. An interesting characteristic of the Danish healthcare system is its decentralization of responsibilities for primary (municipal level) and secondary health care (regional level) provision.
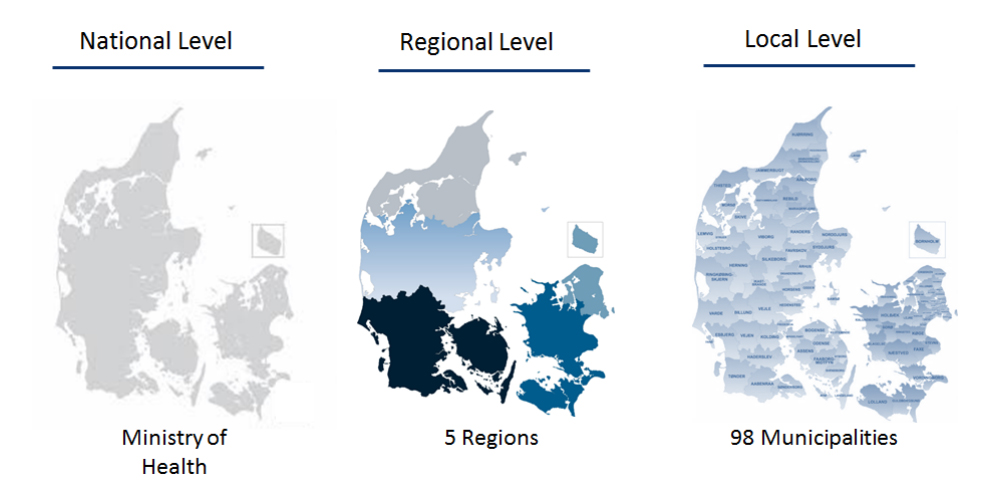
- Nationally, the Ministry of Health, Danish Health Authority, and the Danish Patient Safety Authority are responsible for regulating and supervising all functions related to health. This includes older adults’ care policies, legislation, economic frameworks and quality control. The Danish Health Authority is also responsible for the financing of local health and older adults’ care services such as nursing homes, home care services, and programs for disease prevention, health promotion, and rehabilitation. The Danish Patient Safety Authority is responsible for improving patient safety and quality of care across Danish healthcare.
- There are five administrative regions that manage and finance most public hospitals, hospice care, medical practice sector functioning and social services. These regions must ensure appropriate development through growth initiatives, planning educational offerings and coordinating regional mass transit.
- Denmark has 98 municipalities that are responsible to deliver (with their own methods) services for their residents. Municipalities have to follow quality standards established by the national-level organizations to ensure equal access to health care is independent of where one lives and of economic resources.
7. As long as possible in your own home (Tracey)
As Suelen discussed, Denmark is holding the demand for long-term care steady, while its population of older adults is increasing, by supporting people to remain independent for as long as possible. The supports provided include:
- Preventive visits: These are offered to older adults at set intervals as they age to proactively identify potential care and support needs, and prevent seniors from “falling through the cracks.” Danish municipalities are required by law to offer these visits, and each municipality can design their own processes for doing so. While visits aren’t mandatory, they must be offered, and some don’t take advantage of it. Some municipalities have found that they can increase the acceptance rate by sending out letters with pre-scheduled appointment times to remove the extra step of having to make an appointment.
- Rehabilitation: Short courses of rehabilitation are aimed at restoring or improving skills to remain independent.
- Practical supports: Assistance with tasks like cleaning, laundry, bathing and cooking can help older adults to remain independent.

8. A Danish approach to workforce shortages (Suelen)
Many jurisdictions around the world are facing health-care worker shortages, and Denmark is no exception. When it comes to working with older adults, the country aims to improve the working environment for health-care professionals—making it safer and more appealing to work in.
Denmark also explores innovative technologies as one of the tools to improve the working environment while maintaining a high level of quality care. Ceiling lifts, bathing chairs, reversing systems, sliding and turning systems for beds, entry-exit beds, and hygiene solutions support older adults in their everyday routines, improve professionals’ physical working environment and free up physical and mental resources allowing more time for personal contact and primary care.
9. Conclusion (Tracey and Suelen)
From Saskatchewan to Scandinavia, health and patient care looks a lot different. This is due to a multitude of factors, including but not limited to varying cultural norms, values, geography, history, resourcing and government structure. Rather than focusing on the differences between systems, we—as QI experts—can look to other jurisdictions for their take on health quality and patient care. This was evident at both the conference in Gothenburg and our meetings in Copenhagen. From there, we can use these learnings to establish how changes might look in our own backyard, and work towards them.
Top photo: HQC board member Eugene Paquin (centre), CEO Tracey Sherin (second from right) and researcher Suelen Meira Goes (far right) meet with Laerke Mette Stoltze Kaspersen (far left) and Johanne Andersen Elbek (second from left) from the Danish Health Authority.
Recommended resources
- The Esther project
- Healthcare Denmark whitepaper: A dignified elderly care in Denmark
- Quality improvement at times of crisis




