Masks, social distancing, personal protective equipment, hand-hygiene, vaccines: Navigating the evidence on these topics and more during the COVID-19 pandemic can be an overwhelming task.
In 2020, when the pandemic was first announced, hospitals, long-term care homes, and personal care homes shut their doors to the public across much of the world. When it came time to reopen, provinces varied with regards to if and how visiting restrictions were lifted.
The Canadian Foundation for Healthcare Improvement, now a part of Healthcare Excellence Canada, created the Essential Together program to support organizations across the country re-integrate, welcome, and engage essential care partners as part of care teams, during COVID-19 and beyond.
In this blog, we discuss the Essential Together program, some evidence and recommendations for integrating essential care partners, and some next steps health care organizations and facilities can take to reintegrate essential care partners so patients can have the best outcomes and quality of care.
Table of Contents:
- Essential care partners and their importance
- Successfully reintegrated care partners in the COVID, post-COVID landscape
- International evidence and recommendations on reintegrating care partners
- Reintegrating essential caregivers: Where to go from here
- Let’s work together to make things better
Essential care partners and their importance

Essential Together defines essential care partners as individuals who provide physical, psychological, and emotional support, as deemed important by the patient. This care can include support in decision making, care coordination, and continuity of care. Essential care partners are identified by the patient (or substitute decision maker) and can include family members, close friends or other caregivers. Essential Care Givers, care partners, or designated support people are terms used to explain situations where the resident identifies a consistent person or persons to provide physical or emotional care to them (which may simply mean to spend time with them.) They are provided with training on personal protective equipment, participate in COVID-19 screening, practice hand hygiene and they adhere to other COVID-19 protocols as requested.
The Essential Together program emphasizes that there is a difference between someone who provides physical and emotional support to someone accessing medical care or living in a care facility and a general visitor. Imagine the following situations:
- Being in the hospital and waking up in the emergency department following a car accident and none of your family or loved ones are there.
- Being in a long-term care home and your spouse of 40 years doesn’t live in the home.
- Being alone in an outpatient clinic and you get the results of your MRI, which identifies you have a cancerous brain tumor.
- Being in a group home and your parents are no longer allowed to come to help you with feeding and personal care.
In each of these situations, the person needs physical, psychological, and/or emotional support. Having a loved one present should not be considered “visiting,” as their presence is essential to the well-being of the patient.
It’s important that we ensure essential care partners are not blocked from being present unless the risk is unequivocal in current and future policies. The COVID-19 pandemic has taught us to consider how we can make it safe for essential care givers to be present in health care settings and facilities, just like we do with staff at these facilities.
Successfully reintegrated care partners in the COVID, post-COVID landscape
In 2020, the Essential Together program outlined three foundational principles for the successful reintegration of essential care partners:
- Differentiate between visitors and family caregivers as essential care partners
- Recognize the value of caregivers as essential care partners
- Ensure patients, families, and caregivers have a voice in the development of policies related to visitors and essential care partners
The Essential Together program provides further recommendations and resources that aim to ensure the effective identification and preparation of essential care givers. They encourage having a rapid appeal review process and education programming to ensure safety, infection control and screening protocols are in place.
Recommended reading: Policy Guidance for the Reintegration of Caregivers as Essential Care Partners
International evidence and recommendations on reintegrating care partners

The Essential Together Program also complements international evidence that has emerged since the pandemic began, specifically from the International Long-Term Care (LTC) Policy Network. In 2020, the International LTC Policy Network created a list of recommendations for safe visiting at care homes during COVID-19-based on an international review of best practices and policies. These include:
- Blanket visitor and family caregiver bans should not be used to prevent COVID-19 infections in care homes.
- Safe on-site visiting practices should be used, with options chosen based on local levels of community transmission and in discussion with residents, families and staff and health authorities.
- ‘Family caregivers’ should be designated as essential partners in a resident’s care during the pandemic and be able to have more frequent, longer hands-on visits if they can be supported to do so safely.
- Care homes should receive additional government funding and support to implement safe visiting practices.
- Regulators should be ensuring that care homes meet residents’ rights to have visitors and that safe visiting practices are being used.
The International LTC Policy Network seeks to bring forward the latest information and evidence regarding the impact of COVID-19 in long-term care. The site is useful in understanding the international best practices and key learning that are guiding how families and the public are being re-integrated into long term care homes across the world.
Recommended reading: Safe visiting at care homes during COVID-19: A review of international guidelines and emerging practices during the COVID-19 pandemic
Reintegrating essential caregivers: Where to go from here
As we now look to the possible end of the COVID-19 pandemic, it is critical to ensure that we learn from the pandemic and the evidence that was developed so we can continue to improve the quality of care we offer and receive. In the spirit of continuous improvement, some ways learnings can be applied from Essential Together and International LTC Policy Network in a local context are:
- Policies should be focused on the local context and be based on the level of local transmission and risk. These policies may be built on a tiered system whereby it supports fluctuations due to outbreaks.
- Essential care providers are the same as the general public and should not be considered “visitors.”
- A process should be in place to enable continuity of essential care givers presence in all health care facilities. Education on infection control and personal protective equipment should be provided and screening protocols should be in place.
- Patients, residents, caregivers should be involved in the creation of policies. This includes when restrictions are being imposed and lifted.
- Rapid appeals processes should be in place to address issues that arise in a timely and people-centred manner.
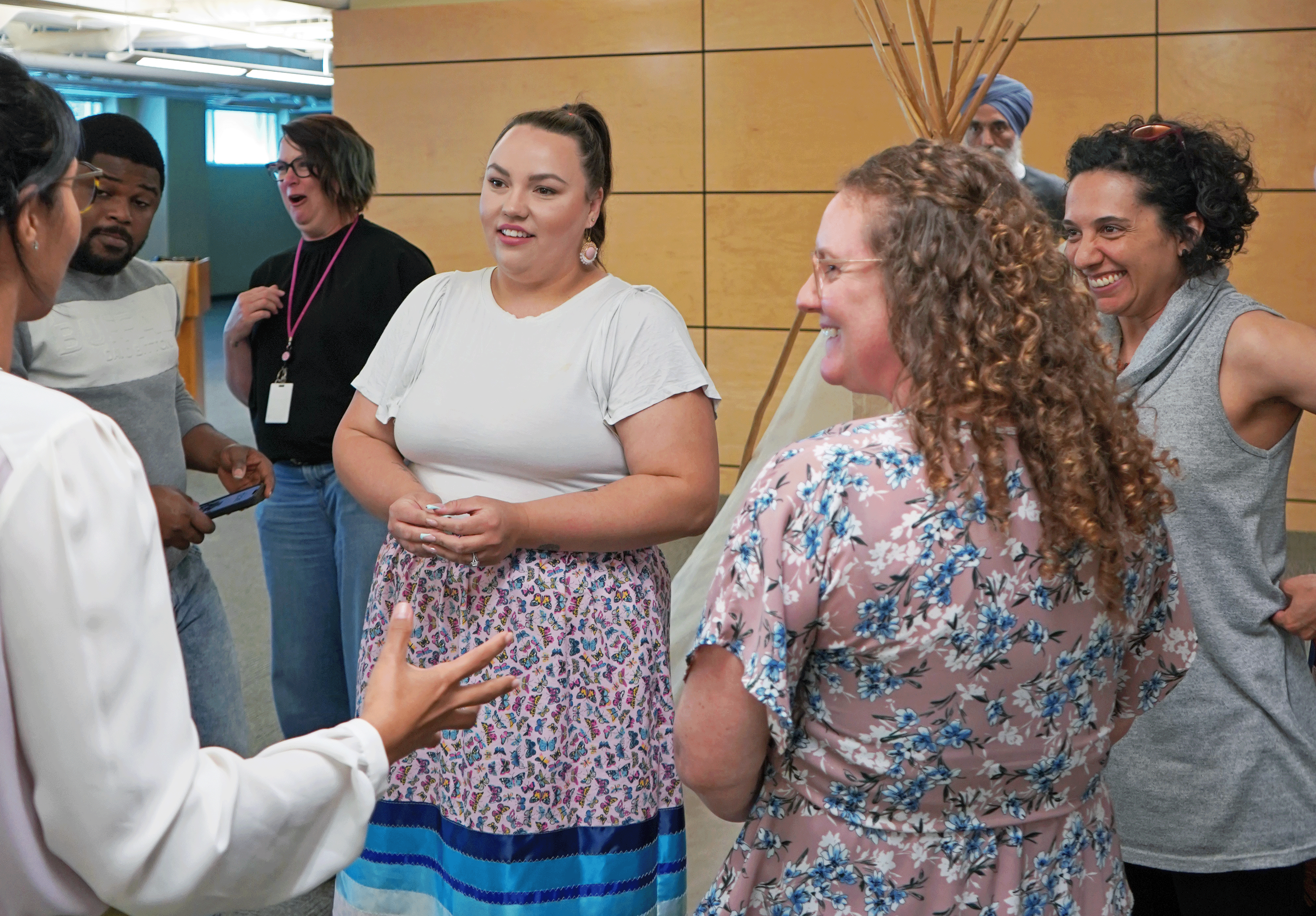
Healthcare Excellence Canada has also launched Essential Together Huddles to bring together those who create, implement, or experience family presence policy during the COVID-19 pandemic and beyond. These 45-minute huddles involve a 15 minute presentation from subject matter experts and/or organizations followed by a group discussion to help encourage peer-to-peer learning and support.
Let’s work together to make things better
The COVID-19 pandemic has enabled us to learn how to do things better. The experience and evidence shows that safe, on-site presence can continue if the local infection and transmission is managed. While limiting public visitation may be necessary, maximizing essential partners support is ideal.
Working together, residents, families, staff, health care facility administrators and authorities can determine what makes the most sense for their environment and while ensuring safety and quality of life for residents.