Panel discussion: How CQIP changed the way I practice medicine
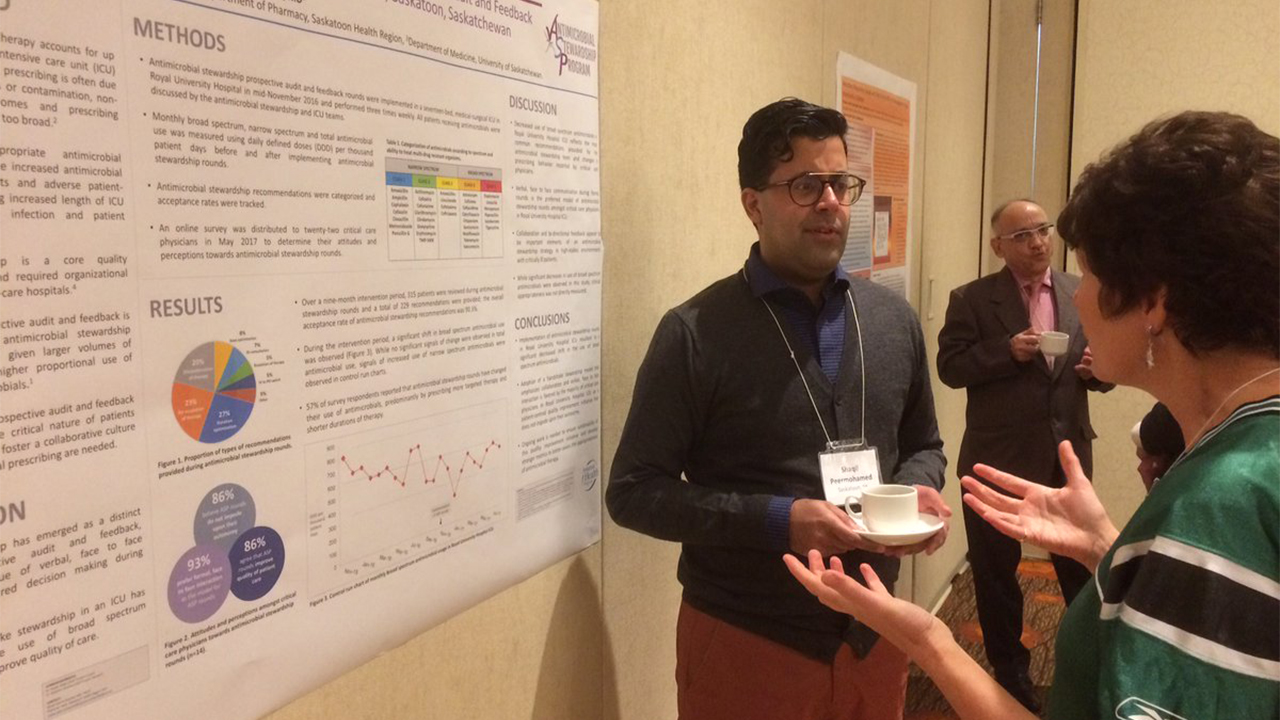
In this post, we feature a panel discussion on the Clinical Quality Improvement Program (CQIP) moderated by Shari Furniss and joined by Dr. Erin Hamilton and Dr. Shaqil Peermohamed. Both Dr. Hamilton and Dr. Peermohamed are graduates of the first cohort of CQIP here in Saskatchewan.
More about our moderator and panel:
- Shari is the Director of Learning and Implementation services at Health Quality Council and has led the development and implementation of the first three waves of CQIP.
- Dr. Shaqil Peermohamed is an infectious disease specialist and physician lead for the antimicrobial stewardship program in Saskatoon, Saskatchewan.
- Dr. Erin Hamilton is a family physician in North Battleford, Saskatchewan.
A brief history of the Clinical Quality Improvement Program in Saskatchewan
Shari Furniss: The Clinical Quality Improvement Program (CQIP) is a sister program to the internationally recognized miniAdvanced Training Program (miniATP), which is offered at Intermountain Health in Utah. The mini-ATP was developed by Dr. Brent James. Intermountain was very welcoming of having us as a sister program and so I want to acknowledge their help and support as we created our own Saskatchewan version. In June 2016, we had a design session to make it a better fit for our Saskatchewan health care system.

At the design session, we had graduates from the Intermountain program, both physicians and non-physicians, graduates of other QI programs such as Quality Improvement Consultant (QIC) School, Clinical Practice Redesign School, Lean Leader or other physician champions, Saskatchewan Medical Association, The Ministry of Health through the Appropriateness of Care work, a representative from our vice president quality group at the time, Health Quality Council and two (absolutely fantastic) patient advisors.
We landed with a program that would help clinicians do clinical quality improvement work, support clinical QI work in the province, and build a network of teachers and coaches and QI champions. The course has these four key theme areas:
- Quality improvement in the Saskatchewan health care system. They’re really looking at some of those tools and methods that are specific to how we work in our province.
- Quality improvement science and methodology. They’re looking at the scientific method based on Deming (W Edwards Deming, creator of the “System of Profound Knowledge”).
- The human side of change. Because all the tools in the world aren’t of much help if you’re not engaging people actively in improvement work.
- A deep dive into clinical QI. Some of the change concepts and ideas that are specific to having a focus on improving appropriateness of clinical care.
What makes CQIP a special program and what makes it resonate is that clinicians are teaching other clinicians. Every participant is paired with a physician coach. We use a flipped classroom methodology so participants complete online modules that are more than theoretical, didactic pieces and then come together for very interactive in-person workshops where they can share and learn from each other. Every participant has a hands-on clinical improvement project to really enrich learning.
After the first cohort, an external program evaluation was done by Dr. Louis Berry. One of themes that emerged from the review was how this has helped people see other opportunities for improvement in their daily work. You can read about the external program evaluation here.
What impact has CQIP had on your work?
Dr. Hamilton: My project focused on increasing HIV testing. I had a few ideas about how we could do this, but as I started the program, I realized that in just offering the HIV test, that’s a simple system. But, how patients interact with the health care system and how we follow up on HIV positive tests is a fairly complex system I don’t think I truly understood as I was going into the project. [Watch Dr. Hamilton’s QIck Talk here.]
Looking back, I think the biggest way CQIP has impacted my work is the idea of systems thinking and seeing problems not just as individual problems but as part of a bigger system. Since participating in CQIP, I’m much more willing to just try something, learn from it, take a first step, know that I don’t understand everything, but see a problem and be curious about it and try something new.
Dr. Peermohamed: Antimicrobial stewardship in and of itself is all about quality improvement. My project was looking at antimicrobial usage in our Critical Care Unit, which is an environment where we can see high rates of broad-spectrum usage. One of the big takeaway messages I got from CQIP was the importance of building relationships, establishing a team, and leading and implementing change. We saw a lot of engagement with the critical care teams. The physicians and pharmacists in the ICU were already starting to think more about their antimicrobial usage for their patients and make some of those changes on their own. There was a lot of empowerment and engagement which was really cool to see. [Watch Dr. Peermohamed’s QIck Talk here.]
What can you tell us about the impact your CQIP project had on patients?
Dr. Peermohamed: I definitely think it has had an impact on patients admitted to the Critical Care Unit. We saw decreased rates of antibiotic usage and decreased usage of inappropriate antimicrobials. In a broader sense, we can see that inappropriate antimicrobial usage is a huge driver of antimicrobial resistance. On a population level, thinking about antimicrobial usage and finding strategies to promote appropriate usage and the right antibiotic for the right patient is absolutely critical.
Another group my project had an impact on was our health care workers. Frontline clinicians, physicians, pharmacists, and nurse practitioners in the Critical Care Unit and beyond are prescribing these agents, so it’s about finding ways to engage and empower them to use the right antibiotic. We also received funding through the College of Medicine to launch a mobile app called Spectrum which has all of the information and more to help promote the right antibiotic based upon Saskatoon’s resistance profiles. We’re hoping with this new quality improvement project, we can take things to a whole new level.
Dr. Hamilton: From my project, we’re hoping that patients don’t have to go and seek out HIV testing and that they’re offered a test when they interact with the health care system. We want it to be something that’s offered to them and they don’t have to seek it out.
The impact that I can see from this project was an instance of two patients that were screened for HIV through walk-in clinic interactions. These patients were there for unrelated reasons. At the walk-in clinic the clinician asked, “Since we’re sending you for blood work, can we add on an HIV test? It’s recommended for every sexually active patient every year.” They said yes and those two patients tested positive and have now been started on antiretrovirals. Those are patients who probably would not have been tested otherwise. We have a project that’s probably going forward to learn more about the patient’s thoughts on being offered the test in different environments.
What did you find helpful for managing some of the challenges with the program?
Dr. Hamilton: One of my biggest challenges was that I made some errors in judgment and scoping of my project in that we probably took on too many areas. What really helped with that was feedback from the network, from the other participants, and from my coach in helping to manage how to best move forward. Networking and working with other participants allowed me to learn about the concepts being applied in very different projects than my own and provided a lot of support and motivation. You would be losing energy to work on your project and then come together for a weekend of learning and go away completely motivated to get back going on your project.
Also, making the time is always a challenge. There are always patient demands and different demands on your time. The coaches and project sponsors were really helpful in helping me figure out how to set aside time and make sure we moved forward.
Where did you start with your project and how did you resize it to be a better fit?
Dr. Hamilton: We started by involving people from every point of contact. We were still in the mindset that we were going to develop a program and we were going to roll it out. As I went through the program, I realized that, no, we need small tests of change starting in some areas and then expand.
Dr. Peermohamed: One thing that I didn’t recognize at the beginning of this project was the importance of having a patient advocate and building that relationship and collaborating with patients when developing a quality improvement project.
How did you involve the patient and what kind of learnings did you have from them that really helped the project?
Dr. Peermohamed: One of our patient advisors was someone who has had multiple admissions in the Critical Care Unit and has several antimicrobial allergies, which makes it very difficult to ensure that she gets the right antibiotic based upon the syndrome that she presents with.
The importance of a stewardship program in the Critical Care Unit is that it ensures continuity. We might have a different lens and know more about some of these patients than some of the Critical Care staff, as we’re used to their histories. This patient also emphasized the importance of letting all patients and families in the Critical Care Unit know about this process and to understand that we’re here to make sure that you’re on the right antibiotic. We’re looking into ways to ensure that patients are aware of this process and families are aware as well.
As alumni of the program, do you have any advice or words of wisdom for other colleagues who are considering applying to CQIP?
Dr. Peermohamed: There are three things that I thought would be key if I were going to do this program again.
- First, it’s really important to be open to ideas. Through CQIP, I was able to collaborate and get advice from so many different people, not just my sponsor and my project supervisor, but others involved in the program. Their feedback helped us evolve our project on an ongoing basis.
- The second thing that I reflected on was the importance of being adaptable and flexible. In quality improvement, we’re looking at thinking about new ways of analyzing data. So rather than creating a research project and looking at P values, maybe a better way to look at things is to run through different PDSA cycles, learn from different interventions, and continue to evolve your process and your project on an ongoing basis.
- The third and final piece of advice that I would give is the importance of collaborating with others. Through CQIP, I was able to build so many connections through SHIPS to help analyze data, to identify patient advocates, to establish better rapport and relationships with the Department of Critical Care as well as the Division of Infectious Diseases and the Department of Pharmacy. Working with my project supervisor Dr. Susan Shaw who works in Critical Care and is also a huge advocate of quality improvement and getting feedback from her was truly amazing.
Dr. Hamilton: I would say the need to pick something meaningful for you and your patients because you do need to have meaning to it to maintain your motivation throughout the year. We all approach problems with some solutions in mind, but as you’re preparing your application, don’t get too attached to your solutions because you get to crowdsource your problems and learn from your patients. We’re never going to get away from having solutions in mind. Just don’t get too attached to your solutions as you’re forming your project and be prepared to learn and change based on what you learn.
One thing I was thinking about is how applicable the project is to both small and large projects. I would encourage any clinicians who are thinking of applying to not feel like you have to be in any kind of leadership or have leadership aspirations to do this program. CQIP is a very helpful program for people who are in leadership or who want to do leadership, but it’s also very, very practical and applicable to your clinical work. Wherever you are on that spectrum, this program can be really valuable.
As CQIP alumni, what is next for you on your QI journey? What’s next for you in terms of quality improvement?
Dr. Hamilton: We’re going to keep working on improving ways of offering HIV testing and probably more patient involvement in all areas of our quality improvement for our clinic because that was another thing that became very clear. It was really striking how much having patients involved both changes and improves the project.
Dr. Peermohamed: We’re continuing our process in the ICU and are continuing to evolve that process as well to make sure it’s as beneficial to critical care staff and patients as well. We’re super excited about the launch of our mobile app which is free for anyone to download and use, and we’ll be continuing to create new clinical guidelines and pathways in Spectrum based upon evidence and also based upon our local resistance patterns.
Can you please talk more about the CQIP training? How long was it and how did it differ from Intermountain?

Shari Furniss: It’s a 10-month program. There are four 2-day workshops and one 1-day workshop in the program. Intermountain is a bit of a shorter program whereas CQIP is spread out over a longer time just to give people more of an opportunity to do more with their projects. CQIP was also designed to incorporate more of the people side of change.
What skills have you learned through your CQIP experience that you’ve found to be most valuable in your day-to-day practice?
Dr. Hamilton: I would say having a range of tool to use. We did some learning around how to run a meeting and how to effectively use huddles and meeting time. As a result, I find a better, more efficient use of my time with my team at our meetings.
Dr. Peermohamed: A huge piece of the work that we do as physicians is quality improvement. When we’re faced with a problem, it’s important to take a step back and reflect in order to identify root causes of that problem and it’s often multifactorial. It’s easy to just create a simple solution, but that may not be effective unless you truly reflect upon all the different causes of an issue and work towards addressing all of the different root causes. That’s one of the things that I have taken away from CQIP as well as using those tools to develop effective solutions. It may be a very multifactorial approach you need to adopt for different issues and that’s okay.
Are the program grads linked to HQC staff to continue providing support if they need it?
Shari Furniss: The short answer is we’re always here if people need us and want to reach out. We love to hear from alumni. We’ve tried to connect folks back into the program so that we can have that ongoing relationship.
Are there other ways that you have been connecting or receiving support post-program?
Dr. Hamilton: By being a coach. It’s kept me connected and I feel pretty comfortable that if I need support to call or email and say, “Hey who can help me with this?” The HQC staff has always been really helpful about providing support and directing me to where I can get help.
Now that you have caught the continuous improvement bug, how do you inspire others you work with who maybe aren’t quite as on-board yet?
Dr. Peermohamed: One way I’ve motivated some of my colleagues to do some quality improvement projects or think about this from a different perspective, is to just reflect upon the patient. At the end of the day, we’re all here to provide effective and optimal care to our patients. It’s always important to keep that as our motivation and our goal. No matter how much work you have to put into this, people will always be receptive to trying to make things better for their patients.
Dr. Hamilton: I would agree with that wholeheartedly. Everybody wants to do a good job for their patients. If we can bring it around to how can we improve care for the patients, most people are on board with that right away. Using the Five Whys with colleagues is helpful for me, but you have to find a different way of phrasing it other than just asking why five times. Being very curious when people are talking about a problem or an area for improvement, trying to ask why do you think that’s a problem, why do you think that problem is there, how could we learn more, and being very curious about their thoughts all helps to engage people.
Applying to participate in CQIP
Shari Furniss: For Saskatchewan clinicians interested in applying for CQIP, I would encourage you to visit the CQIP page to learn more about when applications are due for the next cohort and more information on how to apply. Also, you can follow us on Twitter @CQIP_SK for the latest and greatest CQIP news.