The COVID-19 pandemic has sparked innovation, collaboration and is changing how Saskatchewan health care is delivered. In efforts to keep care safe and accessible, there was an uptick in virtual care. It was invaluable in keeping both physicians and patients safe while maintaining high-quality care.
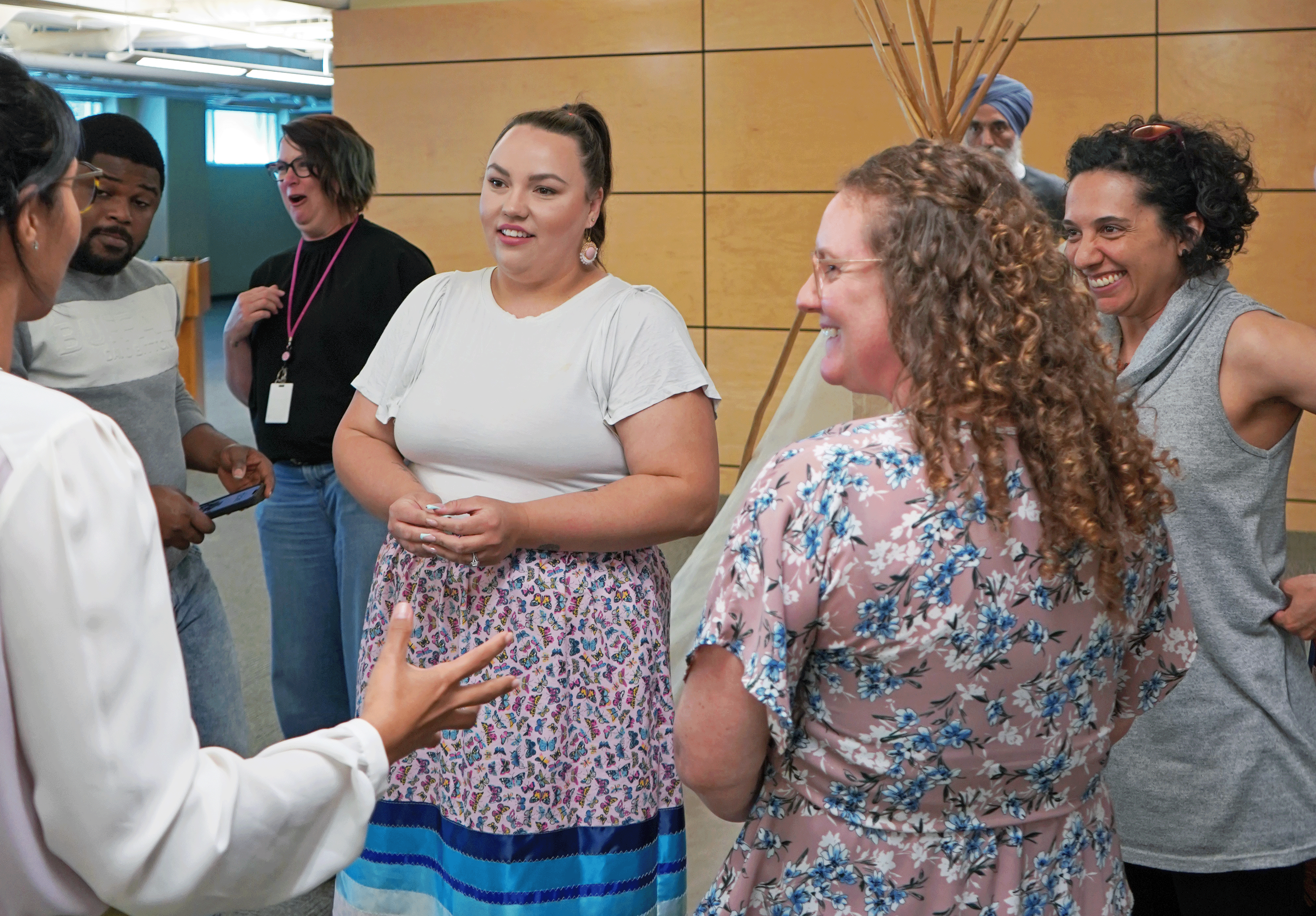
The Saskatchewan Health Quality Council (HQC) brought together a panel of patients and providers to share their experiences and explore virtual care’s impact in the province during a 100-minute panel discussion on Aug. 6, 2020.
Following the event, we asked HQC CEO Tracey Sherin and Moderator Steven Lewis, a health policy and research consultant, to reflect on the webinar by answering these four follow up questions:
- Now that the event has finished, what are your initial thoughts about the information, perspectives, and experiences that were discussed this evening?
- Were there any points that were of a particular interest to you?
- What do you see as the future of virtual care in Saskatchewan?
- How do we apply a QI lens when planning for the future of virtual care in Saskatchewan?
Now that the event has finished, what are your initial thoughts about the information, perspectives, and experiences that were discussed this evening?
Steven Lewis
A couple of things leapt out to me. I expected a little more skepticism, to tell you the truth, and I was pleasantly surprised. As a citizen and patient, I am optimistic of the future of virtual care after hearing that their experiences seem to be almost uniformly good.
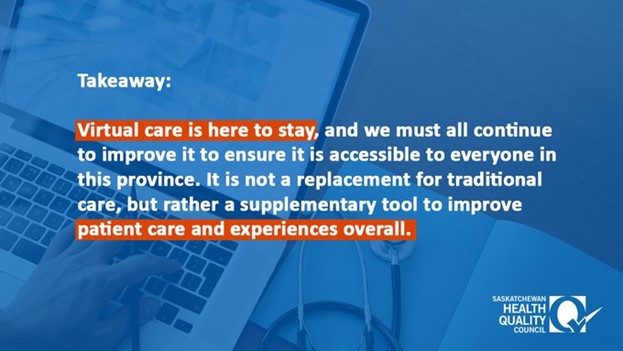
The panelists were thoughtful about their responses. I don’t think the message was to get rid of in-person visits, but it confirmed for me that what has occurred because of circumstance is probably going to be hardwired into the system in the future. Based on what our panelists said, virtual care is going to be a good thing.
Tracey Sherin
Listening to Dr. Janet Tootoosis talk about the team at her clinic getting together and troubleshooting typified quality improvement in action to me. We have a problem we need to solve, we have a theory about how we’re going to solve it, and now we’re testing some changes to do that.
Dr. Tootoosis explained her team did a number of Plan-Do-Study-Act (PDSA) Cycles during the pandemic: “We’ll try this, we learned from that, we’ve identified a gap there, and let’s figure out how to fill that gap.”
That really stood out to me and I think that happened in a lot of different places.
The other piece that stood out to me – and we talked about this when we talked about the definition of virtual care – is that it can be many different things and in many different forms. So we heard Dr. Ivar Mendez talk about robots and assessing patients virtually from across the province. We heard another physician talk about his main tool, which was a telephone, a good old-fashioned phone. So I think there are a lot of opportunities and a lot of different ways that this can look.
A cookie cutter, one-size-fits-all approach probably isn’t going to work and we need to embrace being able to customize care according to different needs and different circumstances.
We heard from five virtual care champions who are leading the way of what good virtual care could look like. This is a great start to the conversation and we need keep this dialogue going to ensure this tool is integrated fully into the system.
Were there any points that were of particular interest to you?
Tracey Sherin
There were a couple that stood out to me. The one was a discussion, and you can relate this back to the dimensions of quality, about appropriateness. The theme that virtual care doesn’t replace other methods of care. Instead, it complements other methods of care and is another tool in the toolbox. I think there will be some experimentation and tinkering, and some evaluation that we’ll have to do to understand how best to deploy that tool with the other tools that we have.
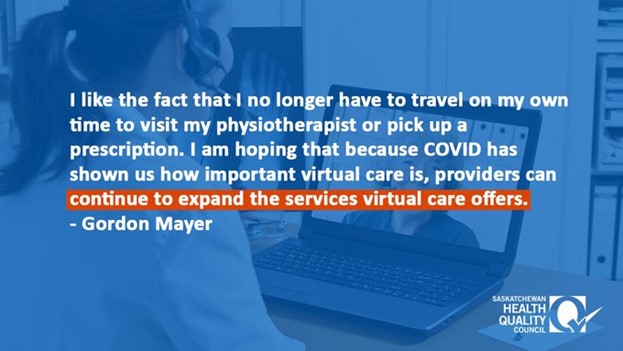
The other point that stood out was the concept of equity. I really resonated with Dr. Tootoosis who talked about digital access as a determinant of health. This is the understanding that while we are increasing access for some, there are still some for whom this is a gap and how it’s not necessarily a health issue, it’s a social determinant of health issue.
Steven Lewis
Building on that a little bit, I’m not sure the jury has decided to what extent in-person care is ever going to be essential.
Of course we think it is essential because that’s what we know, but when you think about a 5G world where we have overcome all of the technological differences in paces of development … all of the technical limitations about zooming in with cameras on very specific parts of the body, combined with other remote technologies such as monitoring devices and so on, I actually think the absolute essential need for hands-on care is going to be extraordinarily limited in the future.
But that will unfold as it unfolds and you don’t have to make that commitment now, you just have to see it coming.
The other thing I was conscious of was the fact that we had the vanguard as the panel. We had two sophisticated Patient Partners and three very thoughtful physicians who think systematically, so it would be interesting to see how far ahead of the general population, both as providers and on the patient side, that they may be.
What do you see as the future of virtual health care in Saskatchewan?
Steven Lewis
I don’t know how ubiquitous it will be in what time frame, but there will be more of it. At least half and probably the greater majority of physicians would say that we’re never going back entirely to the way it was before even if we could.
I think a lot will depend on how much the province willing to invest on the technology – the hardware and the software – to make this work properly.
Secondly, the devil is always in the details: How do you fund health care differently under this model?
Thirdly, how do you attach what we all want to any innovation; how do you make sure that it is really better quality, not just more convenient and more accessible?
I am guardedly optimistic that this will be a very good thing and I virtually have zero concern that it will be an unintendedly bad thing in almost every element. I don’t think there is any significant risk of this causing any harm whatsoever, and there is a significant chance that just improved access and greater intentionality will improve both the process and the outcomes of care.
Maybe not as dramatically as one would hope, but I think this is not only going to be a good thing, but that it might just be the platform that accelerates some of the revolutions that HQC has wanted from day one, which is evidence-based care, more thoughtful adoption of innovation, more rapid jettisoning of obsolete forms of care, and so on.
I see some synergies that could be quite wonderful if this unfolds as the leaders think it should.
Tracey Sherin
To add to that, the future that I would like to see is that virtual care also removes some of the barriers to working across sectors. When you think about the potential of virtual care to increase access and accessibility to health care providers, could it not also increase access and accessibility to multi-sectoral teams of care providers, which could mean your health care provider, social worker, or case worker?
I would like to see virtual care remove some of the barriers to helping multiple sectors collaborate with each other.
How do we apply a QI lens when planning for the future of virtual care in Saskatchewan?
Tracey Sherin
When I think about that, I go back to my first reflection and my grounding in the model for improvement.
I think Steven alluded to this earlier, we have a clear sense of what we are trying to accomplish, we don’t know exactly how we’re going to get there, but we have some idea of the types of changes we’re going to make. Then we will need to measure and monitor as we goto understand whether we’re getting closer or further from that goal.
I think that could serve as a useful model as we go forward because we don’t have a clear path for exactly what is going to happen – we have to figure that out – but we do know where we’re going and we can measure that.
Steven Lewis
This is an innovation and many people have a complicit bias that it’s a work around, that it is the second best thing to the wonderful encounters we have when we go to see the doctor, be in the same room, and have those conversations.
But if something goes wrong and it’s attributed to virtual care, it could undermine confidence in virtual care. So it ups the ante on the evaluation and seeing how this is working, which is a good thing.
I think this is going to add further impetus to evaluating, monitoring, and being very thoughtful about whether we’re measuring the right things and seeing how this works out in the short and long term, all of which are quality improvement adjuncts and foundations.
Health information is actually the foundation of this innovation in a lot of ways and to make it better, we really need to track when it’s used, how it’s used, and what happens when it’s used.
Tracey Sherin
This is where some of our system’s investments in building capacity for quality improvement leadership will start to show us more benefits. So there are physicians who have completed the Clinical Quality Improvement Program (CQIP) for example, who now have the capabilities to lead quality improvement initiatives, so let’s capitalize on those leaders we have out there.
Steven Lewis
Feedback is also important. So you have a virtual visit and let’s say it was 17 minutes and the last two minutes is for an evaluation that takes place immediately following the visit. You have real-time encounter-based evaluation of what is going on, you can switch it up and you can add different modules to those surveys depending on either the characteristics of the patient and so on.
So you would have a feedback mechanism, which is one of the things that even the best of QI has a tough time doing for providers. This would create magnificent opportunities for data collection, painless data supply, and automated kinds of feedback that could be a boon to the whole enterprise.
HQC would like to extend a huge thank you to Tracey Sherin and Steven Lewis for participating in this interview. A recording of the full webinar can be found here.